PERINATAL SAFETY: ROLE OF THE JOINT COMMISSION SAFETY STANDARDS
In this blog, I’ll be reviewing the data trends and leading causes of obstetrical (Ob) related malpractice claims. Additionally, I’ll review identified barriers to adopting evidence-based standards of care while contrasting effective implementation strategies. I’ll conclude with a summary of the 2020 Joint Commission Perinatal Safety Standards and highlight how the required standards align with the Ob related malpractice trends.
Trends / Statistics: The average Ob malpractice payment is $947,000 which is more than twice that of other clinical areas (Crico, 2010). The dollar amount reserved for current and future payment is usually 25% – 35% of the total financial liability cost to the hospital and healthcare system.
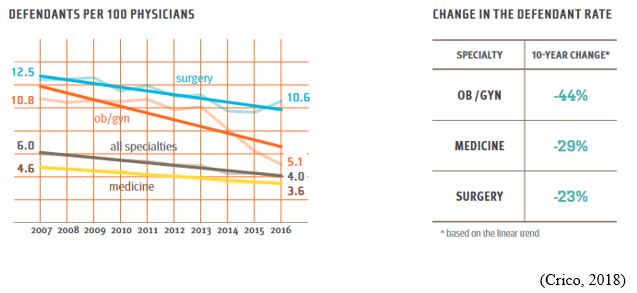
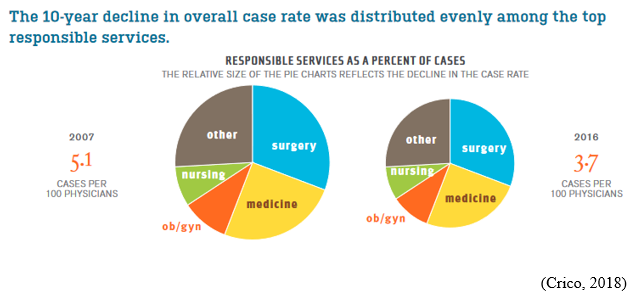
Between 2007-2016, Specific to Ob/Gyns (whose rate is historically higher than the average for all MDs), the risk of having a malpractice case filed against them dropped by 44% (Crico, 2018).
It’s suggested that the drop in claims is a result of quality improvement (QI) initiatives such as training to improve team communication during labor and delivery, and multidisciplinary education on fetal heart rate tracings.
Between 2007-2016, defendant rates declined most steeply in Ob/Gyn. It’s suggested that the declines correlate with long-term safety interventions (Crico, 2018).
There is a risk of permanent and catastrophic damages that can occur as a result of Ob/Gyn medical errors. The Ob/Gyn specialty incurs significantly disproportionate financial losses when compared to the total number of medical malpractices cases.
Most Common Ob Malpractice Claims and Contributing Factors: The majority of Ob related malpractice cases involve birth asphyxia, shoulder dystocia, intrauterine fetal demise and maternal hemorrhage (AWHONN, 2014).
Contributing Factors:
- Clinical judgement: inadequate patient assessment, inappropriate management of pregnancy, failure to timely diagnose and treat a non-reassuring fetal heart rate tracing, inappropriate management of the 2nd stage of labor via operative vaginal birth
- Technical skills: inexperience with procedures
- Communication: provider-provider communication breakdowns, inadequate consent, hierarchical issues
According to FOJP (Hospital Insurance Company), a growing concern has emerged specific to permanent injuries related to shoulder dystocia cases. FOJP found that while clinical judgment factors were trending downward in labor & delivery cases, technical issues were trending upward. The proposed action plan provided was specific to teamwork and simulation training.

It is common knowledge that defensibility is enhanced when care is consistent with current evidence-based standards of care. Despite this knowledge, many organizations continue to struggle with implementing policies, QI and process improvement (PI) initiatives that are consistent with current standards.
Common Barriers to Adopting Evidence-Based Standards of Care:
Leadership Barriers
- Lack of knowledge specific to QI/PI and QI/PI data analysis
- Leadership attitudes
- Leadership practices: not consistently applying new operations, lack of sustainability efforts, lack of time and resources
Clinician Barriers
- Lack of clinician knowledge specific to their own practices, lack of audit & feedback processes, novice status, lack of knowledge about QI/PI projects
- Clinician attitudes: not motivated to change, desires autonomy
- Clinician practices: forgot about QI/PI project, changes add more work or slow down work flow
Characteristics of the QI, or PI Project
- Positive or negative effect on clinician income or time
- Complexity of the QI/PI project
Implementation Climate
- Type of hospital
- Amount of resources
- Type of patients
Strategies for Successful Implementation and Sustainability of Evidence-Based Standards of Care:
Educational strategy: grand rounds, conferences, simulation training, competency tests and demonstrations, on-line learning
Data strategy: audit and feedback methodology to support individual and group data sharing of performance against benchmarks, public release of data focused on outcomes reported openly to the community
Discourse strategy: meetings, review of academic research, reminders via checklists, order sets, newsletters, bulletin boards, emails, rewards for reaching a goal, disciplinary discussions providing feedback specific to performance not aligning with required expectations
How the 2020 Joint Commission Perinatal Safety Standards Align with the Ob Related Malpractice Trends: All hospitals accredited by the Joint Commission are required to comply with the 2020 Joint Commission Perinatal Safety Standards. The safety standards were developed in response to the leading causes of perinatal morbidity and mortality: maternal hemorrhage and severe hypertension/preeclampsia.
A number of the required elements of performance center around:
- The development of written evidence-based procedures for managing Ob emergency events (educational and discourse strategy).
- Providing role-specific education to all staff and providers who treat pregnant and postpartum patients about the organization’s procedures at a minimum every two years (educational strategy).
- Supporting annual multidisciplinary simulation drills to determine system issues as a part of on-going QI efforts (educational strategy).
- Completing regular reviews of severe maternal morbidity and mortality cases to evaluate effectiveness of the care, treatment, and services provided by the response team during the event (data strategy).
Knowledge is power, power is change. We, as a multidisciplinary group of clinicians, and legal representatives, need to be the change we wish to see by propelling healthcare policies that are consistent with current evidence-based standards.
References
AWHONN, 2014. Perinatal Nursing 4th ed.
AWHONN, 2021. Perinatal Nursing 5th ed.
Crico, 2010. CBS Benchmarking Report – Medical Malpractice in America
Crico, 2018. CBS Benchmarking Report – Medical Malpractice in America
The Joint Commission, 2019. Provision of Care, Treatment, and Services standards for maternal safety
P.S. Comment and Share: Have you been involved in developing and/or implementing a new perinatal policy, QI, or PI initiative in response to the 2020 Joint Commission Perinatal Safety Standards? If so, what was the policy/QI/PI initiative and how has it improved outcomes?
Leave a Reply