SIGNIFICANCE OF A SINUSOIDAL FETAL HEART RATE (FHR) PATTERN
Case Review: 21-year-old primiparous (first pregnancy) at 35+4 weeks gestational age presents to labor and delivery triage status post a motor vehicle accident (MVA) 4 hours prior to arrival. Patient reports occasional mild uterine contractions on arrival. Denies vaginal bleeding, or leaking of fluid. Reports decreased fetal movement since the MVA. Obstetrical history is significant for anemia, and O negative blood type.
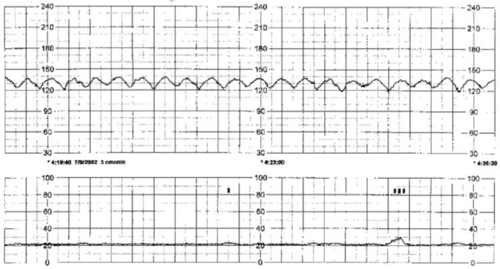
1:30pm: RN progress note – occasional mild uterine contractions. Abdomen soft, non-tender. FHR 125 with moderate variability. Occasional accelerations. Absent decelerations. Occasional mild uterine contractions. Category I fetal heart rate (FHR) tracing reported to attending Ob/Gyn via telephone (in reference to above tracing).
5:30pm: RN progress note – Telephone report provided to Dr. Z. Category I tracing. Reassuring maternal, and fetal status. Rhogam administered. Orders received to discharge patient home with follow up in office as previously scheduled.
11:30pm: Patient returned to labor and delivery triage with onset of painful uterine contractions, and vaginal bleeding. Uncertain if perceiving fetal movement. Abdomen rigid, and tender to touch. Fetal heart tones absent. Intrauterine fetal demise confirmed via bedside obstetrical ultrasound. Patient desires primary cesarean section. Placenta abruption confirmed at delivery.
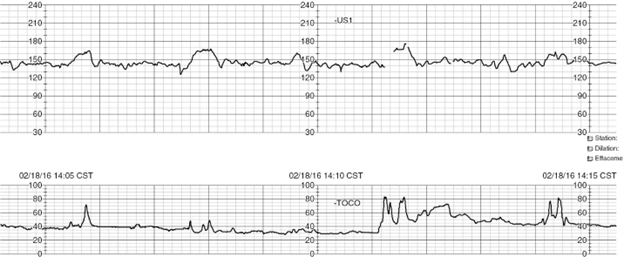
Sinusoidal FHR Pattern: A sinusoidal FHR pattern is uncommon. The smooth, sine wave-like undulating pattern in the FHR baseline serves to distinguish this pattern from variability. In the presence of a sinusoidal FHR pattern, there is a cycle frequency of 3 to 5 per minute that persists for 20 minutes. A sinusoidal FHR pattern can be misinterpreted as moderate variability. This misinterpretation puts the team (including the patient, and her family) at risk for misdiagnosis, and mismanagement.
An effective way to distinguish FHR variability from the sinusoidal pattern is by recognizing that variability is defined as fluctuations in the baseline that are irregular in amplitude, and frequency. By contrast, the sinusoidal pattern is characterized by fluctuations in the baseline that are regular in amplitude, and frequency. Spontaneous accelerations are absent, nor are they elicited in response to uterine contractions, fetal movement, or stimulation (i.e., digital scalp stimulation, vibroacoustic stimulation).
Causes: Causes of a sinusoidal FHR pattern can include fetal anemia as a result of Rh isoimmunization (i.e., the mother’s blood protein is incompatible with the fetus’s in the case of a maternal Rh negative [O negative] blood type), fetal maternal hemorrhage (i.e., placenta abruption), twin-to-twin transfusion syndrome, ruptured vasa previa, and fetal intracranial hemorrhage. Other fetal conditions that have been reported to be associated with a sinusoidal FHR pattern include fetal hypoxia or asphyxia, fetal infection, fetal cardiac anomalies, and gastroschisis.
Pseudosinusoidal, or medication induced sinusoidal can occur after the administration of some opioids, fetal sleep cycles, or rhythmical movements of the fetal mouth. These events are of short duration, preceded, and followed by an FHR with normal characteristics. These short periods of sinusoidal appearing patterns do not require treatment.
Significance / Management: A sinusoidal FHR pattern is associated with an increased risk for fetal acidemia at the time of observation. This pattern is to be considered a Category III (abnormal), which requires immediate evaluation, intrauterine resuscitation, and expedited birth if unresolved.
References
Lydon, and Wisner, (2021). Fetal Heart Monitoring Principles and Practices
Miller et al., (2022). Mosby’s Pocket Guide to Fetal Monitoring
Simpson et al., (2021). Perinatal Nursing
P.S. COMMENT AND SHARE: What is your experience reviewing a case involving a sinusoidal FHR pattern? Was the abnormal pattern identified timely? Was the pattern misinterpreted as moderate variability? What was the neonatal outcome?