THE ROLE SICKLE CELL DISEASE HAS ON MATERNAL, FETAL & NEONATAL MORBIDITY & MORTALITY: IMPORTANCE OF CAREFUL CAUSAL CONNECTION
What is Sickle Cell Disease (SCD): SCD is a group of inherited red blood cell disorders that affect hemoglobin, the protein that carries oxygen throughout the body.
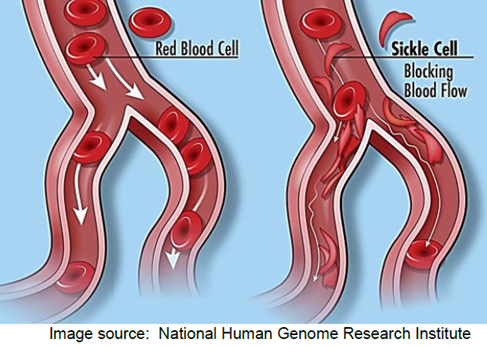
Normally, red blood cells are disc-shaped and flexible enough to move easily through the blood vessels. If you have sickle cell disease, your red blood cells are crescent, or “sickle” shaped. These cells do not bend or move easily and can block blood flow to the rest of your body.
The blocked blood flow through the body can lead to serious problems, including stroke, eye problems, infections, and episodes of pain called pain crises.
Maternal, Fetal and Neonatal Risks Associated with SCD: There is increased maternal and fetal morbidity and mortality associated with SCD. There is an increased risk for hypertensive disorders of pregnancy. For example, the rate of preeclampsia in pregnant women with SCD is approximately 1 in 8 (12%). Women with SCD also have an increased risk of gestational hypertension (JAMA Pediatrics, 2023). Additionally, there is an increased risk for venous thromboembolisms (blood clots), increased pain, worsening anemia, worsening kidney and liver disease, poor fetal growth, preterm labor, and fetal loss. Newborns are more likely to have growth problems and suffer from the associated complications of prematurity.
Statistics: SCD affects more than 100,000 people in the United States and 20 million people worldwide (NIH). Based on review of a recent retrospective cohort study published in JAMA Pediatrics (2023), women with SCD had a maternal mortality rate of 14 per 10,000 deliveries compared with 1 per 10,000 deliveries among women without SCD. SCD complicated 0.37% of pregnancies studied, but contributed to 4.3% – 6.9% of the severe maternal morbidity cases dependent on red blood cell transfusion status.
In economically advanced countries the rate of fetal and neonatal death is as high as 2.9 per 1,000 deliveries. There is a five-fold increase in fetal and neonatal deaths in less resourced countries (Hematology, 2019).
Pregnancy Management: There are very few therapeutic interventions that have been studied other than prophylactic and selective blood transfusion therapy to improve perinatal outcomes. Due to the increased risk of hypertensive disorders in pregnancy and venous thromboembolism associated with SCD, low-dose aspirin prophylaxis (81 mg per day) is recommended between 12 – 28 weeks of gestation for those women with no contraindications to aspirin. Aspirin therapy should be continued until the time of delivery (ACOG, 2022).
Additionally, ACOG (2022) recommends universal hemoglobinopathy testing in women planning pregnancy or at the initial prenatal visit if no prior testing results are available. This testing supports pre-pregnancy, or prenatal diagnosis, genetic counseling and learning of reproductive options early. Hemoglobinopathy testing may be performed using hemoglobin electrophoresis or molecular genetic testing.
ACOG (2022) recommends that women of reproductive-age with SCD who have a personal history of pulmonary embolism or signs / symptoms of hypoxia undergo screening with transthoracic Doppler echocardiography due to the increased risk of pulmonary hypertension. For patients with symptoms, a screening echocardiogram before pregnancy is recommended. Further evaluation, including right heart catheterization, is ideally performed prior to pregnancy. High risk findings, such as pulmonary arterial hypertension (PAH) may impact the advisability of pregnancy. However, if a screening echocardiogram cannot be obtained prior to pregnancy, it can be performed in early pregnancy. Abnormal echocardiographic findings should be co-managed by a multidisciplinary team, including consultants with expertise in SCD.
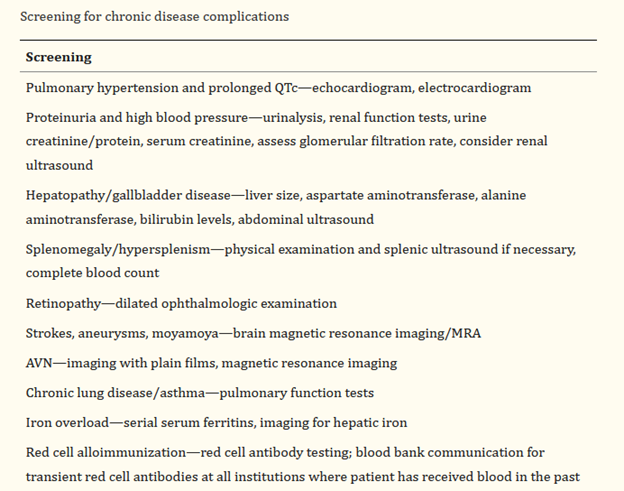
(Hematology, 2019)
Review of Causal Connection in Maternal, Fetal and Neonatal Death Cases Complicated by SCD: Causation in a medical liability claim is crucial in order to establish recovery. The claimant, or defendant, must prove 1) the existence of a duty; 2) a breach of that duty; 3) injury or damages to the claimant; and 4) a causal connection between the breach of duty and the alleged injuries. Causation issues must be carefully considered and are established by reasonable medical probability (a reasonable degree of medical certainty). This requires showing that the injury was more likely than not caused by a particular stimulus, act, or omission of care based on the standards of care.
It’s crucial to get the correct experts involved in case review and development to ensure that all aspects of causal connection have been evaluated. Working with experts who are aware of the pathophysiology of CSD, associated maternal, fetal and neonatal co-morbidities, as well as management recommendations will support the evaluation of causation.
Resources:
ACOG, 2022. Hemoglobinopathies in Pregnancy
Hematology, American Society of Hematology Education Program, 2019. Complications in Pregnant Women with Sickle Cell Disease.
JAMA Pediatrics, 2023. Association of SCD with Racial Disparities and Severe Maternal Morbidities in Black Individuals
The National Institute of Health
P.S. Comment and Share: What is your experience with SCD? Did your role require you to evaluate causal connection between SCD and maternal, fetal or neonatal injury, or death?